Pre-Action Protocol for the Resolution of Clinical Disputes Clinical Disputes Forum
Contents
1 INTRODUCTION
1.1 This Protocol is intended to apply to all claims against hospitals, GPs, dentists and other healthcare providers (both NHS and private) which involve an injury that is alleged to be the result of clinical negligence. It is not intended to apply to claims covered by—
(a) the Pre-Action Protocol for Disease and Illness Claims;
(b) the Pre-Action Protocol for Personal Injury Claims;
(c) the Pre-Action Protocol for Low Value Personal Injury Claims in Road Traffic Accidents;
(d) the Pre-Action Protocol for Low Value Personal Injury (Employers’ Liability and Public Liability) Claims; or
(e) Practice Direction 3D – Mesothelioma Claims
1.2 This Protocol is intended to be sufficiently broad-based and flexible to apply to all sectors of healthcare, both public and private. It also recognises that a claimant and a defendant, as patient and healthcare provider, may have an ongoing relationship.
1.3 It is important that each party to a clinical dispute has sufficient information and understanding of the other’s perspective and case to be able to investigate a claim efficiently and, where appropriate, to resolve it. This Protocol encourages a cards-on-the-table approach when something has gone wrong with a claimant’s treatment or the claimant is dissatisfied with that treatment and/or the outcome.
1.4 This Protocol is now regarded by the courts as setting the standard of normal reasonable pre-action conduct for the resolution of clinical disputes.
1.5
1.5.1 This Protocol sets out the conduct that prospective parties would normally be expected to follow prior to the commencement of any proceedings. It establishes a reasonable process and timetable for the exchange of information relevant to a dispute, sets out the standards for the content and quality of letters of claim and sets standards for the conduct of pre-action negotiations.
1.5.2 The timetable and the arrangements for disclosing documents and obtaining expert evidence may need to be varied to suit the circumstances of the case. Where one or more parties consider the detail of the Protocol is not appropriate to the case, and proceedings are subsequently issued, the court will expect an explanation as to why the Protocol has not been followed, or has been varied.
Early Issue
1.6
1.6.1 The Protocol provides for a defendant to be given four months to investigate and respond to a Letter of Claim before proceedings are served. If this is not possible, the claimant’s solicitor should give as much notice of the intention to issue proceedings as is practicable. This Protocol does not alter the statutory time limits for starting court proceedings. If a claim is issued after the relevant statutory limitation period has expired, the defendant will be entitled to use that as a defence to the claim. If proceedings are started to comply with the statutory time limit before the parties have followed the procedures in this Protocol, the parties should apply to the court for a stay of the proceedings while they so comply.
1.6.2 The parties should also consider whether there is likely to be a dispute as to limitation should a claim be pursued.
Enforcement of the Protocol and sanctions
1.7 Where either party fails to comply with this Protocol, the court may impose sanctions. When deciding whether to do so, the court will look at whether the parties have complied in substance with the Protocol’s relevant principles and requirements. It will also consider the effect any non-compliance has had on any other party. It is not likely to be concerned with minor or technical shortcomings (see paragraph 4.3 to 4.5 of the Practice Direction on Pre-Action Conduct and Protocols).
Litigants in Person
1.8 If a party to a claim does not seek professional advice from a solicitor they should still, in so far as is reasonably possible, comply with the terms of this Protocol. In this Protocol “solicitor” is intended to encompass reference to any suitably legally qualified person.
If a party to a claim becomes aware that another party is a litigant in person, they should send a copy of this Protocol to the litigant in person at the earliest opportunity.
2 THE AIMS OF THE PROTOCOL
2.1 The general aims of the Protocol are –
(a) to maintain and/or restore the patient/healthcare provider relationship in an open and transparent way;
(b) to reduce delay and ensure that costs are proportionate; and
(c) to resolve as many disputes as possible without litigation.
2.2 The specific objectives are–
(a) to encourage openness, transparency and early communication of the perceived problem between patients and healthcare providers;
(b) to provide an opportunity for healthcare providers to identify whether notification of a notifiable safety incident has been, or should be, sent to the claimant in accordance with the duty of candour imposed by section 20 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014;
(c) to ensure that sufficient medical and other information is disclosed promptly by both parties to enable each to understand the other’s perspective and case, and to encourage early resolution or a narrowing of the issues in dispute;
(d) to provide an early opportunity for healthcare providers to identify cases where an investigation is required and to carry out that investigation promptly;
(e) to encourage healthcare providers to involve the National Health Service Litigation Authority (NHSLA) or their defence organisations or insurers at an early stage;
(f) to enable the parties to avoid litigation by agreeing a resolution of the dispute;
(g) to enable the parties to explore the use of mediation or to narrow the issues in dispute before proceedings are commenced;
(h) to enable parties to identify any issues that may require a separate or preliminary hearing, such as a dispute as to limitation;
(i) to support the efficient management of proceedings where litigation cannot be avoided;
(j) to discourage the prolonged pursuit of unmeritorious claims and the prolonged defence of meritorious claims;
(k) to promote the provision of medical or rehabilitation treatment to address the needs of the claimant at the earliest opportunity; and
(l) to encourage the defendant to make an early apology to the claimant if appropriate.
2.3 This Protocol does not—
(a) provide any detailed guidance to healthcare providers on clinical risk management or the adoption of risk management systems and procedures;
(b) provide any detailed guidance on which adverse outcomes should trigger an investigation; or
(c) recommend changes to the codes of conduct of professionals in healthcare.
3 THE PROTOCOL
3.1 An illustrative flowchart is attached at Annex A which shows each of the stages that the parties are expected to take before the commencement of proceedings.
Obtaining health records
3.2 Any request for records by the claimant should–
(a) provide sufficient information to alert the defendant where an adverse outcome has been serious or has had serious consequences or may constitute a notifiable safety incident;
(b) be as specific as possible about the records which are required for an initial investigation of the claim (including, for example, a continuous copy of the CTG trace in birth injury cases); and
(c) include a request for any relevant guidelines, analyses, protocols or policies and any documents created in relation to an adverse incident, notifiable safety incident or complaint.
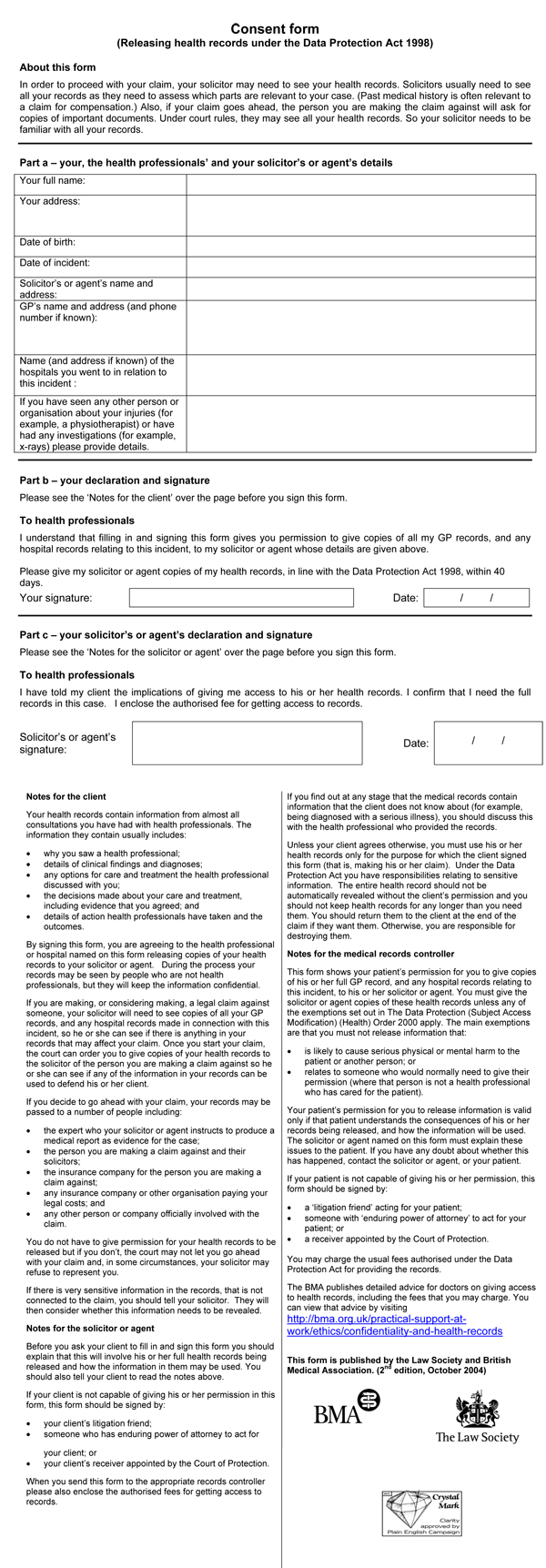
3.3 Requests for copies of the claimant’s clinical records should be made using the Law Society and Department of Health approved standard forms (enclosed at Annex B), adapted as necessary.
3.4
3.4.1 The copy records should be provided within 40 days of the request and for a cost not exceeding the charges permissible under the Access to Health Records Act 1990 and/or the Data Protection Act 1998. Payment may be required in advance by the healthcare provider.
3.4.2 The claimant may also make a request under the Freedom of Information Act 2000.
3.5 At the earliest opportunity, legible copies of the claimant’s medical and other records should be placed in an indexed and paginated bundle by the claimant. This bundle should be kept up to date.
3.6 In the rare circumstances that the defendant is in difficulty in complying with the request within 40 days, the problem should be explained quickly and details given of what is being done to resolve it.
3.7 If the defendant fails to provide the health records or an explanation for any delay within 40 days, the claimant or their adviser can then apply to the court under rule 31.16 of the Civil Procedure Rules 1998 (‘CPR’) for an order for pre-action disclosure. The court has the power to impose costs sanctions for unreasonable delay in providing records.
3.8 If either the claimant or the defendant considers additional health records are required from a third party, in the first instance these should be requested by or through the claimant. Third party healthcare providers are expected to co-operate. Rule 31.17 of the CPR sets out the procedure for applying to the court for pre-action disclosure by third parties.
Rehabilitation
3.9 The claimant and the defendant shall both consider as early as possible whether the claimant has reasonable needs that could be met by rehabilitation treatment or other measures. They should also discuss how these needs might be addressed. An immediate needs assessment report prepared for the purposes of rehabilitation should not be used in the litigation except by consent.
(A copy of the Rehabilitation Code can be found at: http://www.iua.co.uk/IUA_Member/Publications (opens in a new tab))
Letter of Notification
3.10 Annex C1 to this Protocol provides a template for the recommended contents of a Letter of Notification; the level of detail will need to be varied to suit the particular circumstances.
3.11
3.11.1 Following receipt and analysis of the records and, if appropriate, receipt of an initial supportive expert opinion, the claimant may wish to send a Letter of Notification to the defendant as soon as practicable.
3.11.2 The Letter of Notification should advise the defendant that this is a claim where a Letter of Claim is likely to be sent because a case as to breach of duty and/or causation has been identified. A copy of the Letter of Notification should also be sent to the NHSLA or, where known, other relevant medical defence organisation or indemnity provider.
3.12
3.12.1 On receipt of a Letter of Notification a defendant should—
(a) acknowledge the letter within 14 days of receipt;
(b) identify who will be dealing with the matter and to whom any Letter of Claim should be sent;#
(c) consider whether to commence investigations and/or to obtain factual and expert evidence;
(d) consider whether any information could be passed to the claimant which might narrow the issues in dispute or lead to an early resolution of the claim; and
(e) forward a copy of the Letter of Notification to the NHSLA or other relevant medical defence organisation/indemnity provider.
3.12.2 The court may question any requests by the defendant for extension of time limits if a Letter of Notification was sent but did not prompt an initial investigation.
Letter of Claim
3.13 Annex C2 to this Protocol provides a template for the recommended contents of a Letter of Claim: the level of detail will need to be varied to suit the particular circumstances.
3.14 If, following the receipt and analysis of the records, and the receipt of any further advice (including from experts if necessary – see Section 4), the claimant decides that there are grounds for a claim, a letter of claim should be sent to the defendant as soon as practicable. Any letter of claim sent to an NHS Trust should be copied to the National Health Service Litigation Authority.
3.16 This letter should contain—
(a) a clear summary of the facts on which the claim is based, including the alleged adverse outcome, and the main allegations of negligence;
(b) a description of the claimant’s injuries, and present condition and prognosis;
(c) an outline of the financial loss incurred by the claimant, with an indication of the heads of damage to be claimed and the scale of the loss, unless this is impracticable;
(d) confirmation of the method of funding and whether any funding arrangement was entered into before or after April 2013; and
(e) the discipline of any expert from whom evidence has already been obtained.
3.17 The Letter of Claim should refer to any relevant documents, including health records, and if possible enclose copies of any of those which will not already be in the potential defendant’s possession, e.g. any relevant general practitioner records if the claimant’s claim is against a hospital.
3.18 Sufficient information must be given to enable the defendant to focus investigations and to put an initial valuation on the claim.
3.19 Letters of Claim are not intended to have the same formal status as Particulars of Claim, nor should any sanctions necessarily apply if the Letter of Claim and any subsequent Particulars of Claim in the proceedings differ.
3.20 Proceedings should not be issued until after four months from the letter of claim.
In certain instances it may not be possible for the claimant to serve a Letter of Claim more than four months before the expiry of the limitation period. If, for any reason, proceedings are started before the parties have complied, they should seek to agree to apply to the court for an order to stay the proceedings whilst the parties take steps to comply.
3.21 The claimant may want to make an offer to settle the claim at this early stage by putting forward an offer in respect of liability and/or an amount of compensation in accordance with the legal and procedural requirements of CPR Part 36 (possibly including any costs incurred to date). If an offer to settle is made, generally this should be supported by a medical report which deals with the injuries, condition and prognosis, and by a schedule of loss and supporting documentation. The level of detail necessary will depend on the value of the claim. Medical reports may not be necessary where there is no significant continuing injury and a detailed schedule may not be necessary in a low value case.
Letter of Response
3.22 Attached at Annex C3 is a template for the suggested contents of the Letter of Response: the level of detail will need to be varied to suit the particular circumstances.
3.23 The defendant should acknowledge the Letter of Claim within 14 days of receipt and should identify who will be dealing with the matter.
3.24 The defendant should, within four months of the Letter of Claim, provide a reasoned answer in the form of a Letter of Response in which the defendant should—
(a) if the claim is admitted, say so in clear terms;
(b) if only part of the claim is admitted, make clear which issues of breach of duty and/or causation are admitted and which are denied and why;
(c) state whether it is intended that any admissions will be binding;
(d) if the claim is denied, include specific comments on the allegations of negligence and, if a synopsis or chronology of relevant events has been provided and is disputed, the defendant’s version of those events;
(e) if supportive expert evidence has been obtained, identify which disciplines of expert evidence have been relied upon and whether they relate to breach of duty and/or causation;
(f) if known, state whether the defendant requires copies of any relevant medical records obtained by the claimant (to be supplied for a reasonable copying charge);
(g) provide copies of any additional documents relied upon, e.g. an internal protocol;
(h) if not indemnified by the NHS, supply details of the relevant indemnity insurer; and
(i) inform the claimant of any other potential defendants to the claim.
3.25
3.25.1 If the defendant requires an extension of time for service of the Letter of Response, a request should be made as soon as the defendant becomes aware that it will be required and, in any event, within four months of the letter of claim.
3.25.2 The defendant should explain why any extension of time is necessary.
3.25.3 The claimant should adopt a reasonable approach to any request for an extension of time for provision of the reasoned answer.
3.26 If the claimant has made an offer to settle, the defendant should respond to that offer in the Letter of Response, preferably with reasons. The defendant may also make an offer to settle at this stage. Any offer made by the defendant should be made in accordance with the legal and procedural requirements of CPR Part 36 (possibly including any costs incurred to date). If an offer to settle is made, the defendant should provide sufficient medical or other evidence to allow the claimant to properly consider the offer. The level of detail necessary will depend on the value of the claim.
3.27 If the parties reach agreement on liability, or wish to explore the possibility of resolution with no admissions as to liability, but time is needed to resolve the value of the claim, they should aim to agree a reasonable period.
3.28 If the parties do not reach agreement on liability, they should discuss whether the claimant should start proceedings and whether the court might be invited to direct an early trial of a preliminary issue or of breach of duty and/or causation.
3.29 Following receipt of the Letter of Response, if the claimant is aware that there may be a delay of six months or more before the claimant decides if, when and how to proceed, the claimant should keep the defendant generally informed.
4 EXPERTS
4.1 In clinical negligence disputes separate expert opinions may be needed—
- on breach of duty;
- on causation;
- on the patient’s condition and prognosis;
- to assist in valuing aspects of the claim.
4.2 It is recognised that in clinical negligence disputes, the parties and their advisers will require flexibility in their approach to expert evidence. The parties should co-operate when making decisions on appropriate medical specialisms, whether experts might be instructed jointly and whether any reports obtained pre-action might be shared.
4.3 Obtaining expert evidence will often be an expensive step and may take time, especially in specialised areas of medicine where there are limited numbers of suitable experts.
4.4 When considering what expert evidence may be required during the Protocol period, parties should be aware that the use of any expert reports obtained pre-action will only be permitted in proceedings with the express permission of the court.
5 ALTERNATIVE DISPUTE RESOLUTION
5.1 Litigation should be a last resort. As part of this Protocol, the parties should consider whether negotiation or some other form of alternative dispute resolution (‘ADR’) might enable them to resolve their dispute without commencing proceedings.
5.2 Some of the options for resolving disputes without commencing proceedings are—
(a) discussion and negotiation (which may or may not include making Part 36 Offers or providing an explanation and/or apology)
(b) mediation, a third party facilitating a resolution ;
(c) arbitration, a third party deciding the dispute;
(d) early neutral evaluation, a third party giving an informed opinion on the dispute; and
(e) Ombudsmen schemes.
5.3 Information on mediation and other forms of ADR is available in the Jackson ADR Handbook (available from Oxford University Press) or at—
https://www.gov.uk/guidance/a-guide-to-civil-mediation (opens in a new tab)
5.4 If proceedings are issued, the parties may be required by the court to provide evidence that ADR has been considered. It is expressly recognised that no party can or should be forced to mediate or enter into any form of ADR, but a party’s silence in response to an invitation to participate in ADR might be considered unreasonable by the court and could lead to the court ordering that party to pay additional court costs.
6 STOCKTAKE
6.1
6.1.1 Where a dispute has not been resolved after the parties have followed the procedure set out in this Protocol, the parties should review their positions before the claimant issues court proceedings.
6.1.2 If proceedings cannot be avoided, the parties should continue to co-operate and should seek to prepare a chronology of events which identifies the facts or issues that are agreed and those that remain in dispute. The parties should also seek to agree the necessary procedural directions for efficient case management during the proceedings.
Annex A
ILLUSTRATIVE FLOWCHART
DownloadIllustrative flowchart (PDF, 108 KB)
Annex B
FORM FOR REQUESTING MEDICAL RECORDS
Annex C
TEMPLATES FOR LETTERS OF NOTIFICATION, CLAIM AND RESPONSE
C1 Letter of Notification
Letter of Notification
Re: [Claimant’s Name, Address, DoB and NHS Number]
We have been instructed to act on behalf of [Claimant’s name] in relation to treatment carried out/care provided at [name of hospital or treatment centre] by [name of clinician(s) if known] on [insert date(s)].
The purpose of this letter is to notify you that, although we are not yet in a position to serve a formal Letter of Claim, our initial investigations indicate that a case as to breach of duty and/or causation has been identified. We therefore invite you to commence your own investigation and draw your attention to the fact that failure to do may be taken into account when considering the reasonableness of any subsequent application for an extension of time for the Letter of Response.
We understand that you are the correct defendant in respect of treatment provided by [name of clinician] at [hospital/surgery/treatment centre] on [date(s)]. If you do not agree, please provide us with any information you have that may assist us to identify the correct defendant. Failure to do so may result in costs sanctions should proceedings be issued.
Summary of Facts and Alleged Adverse Outcome
[Outline what is alleged to have happened and provide a chronology of events with details of relevant known treatment/care.]
[Provide index of records obtained and request for further records/information if required.]
Allegations of Negligence
[Brief outline of any alleged breach of duty and causal link with any damage suffered.]
Expert Evidence
[State whether expert evidence has been obtained or is awaited and, if so, the relevant discipline.]
Damage
[Brief outline of any injuries attributed to the alleged negligence and their functional impact.]
Funding
[If known, state method of funding and whether arrangement was entered into before or after April 2013.]
Rehabilitation
As a result of the allegedly negligent treatment, our client has injuries/needs that could be met by rehabilitation. We invite you to consider how this could be achieved.
Limitation
For the purposes of limitation, we calculate that any proceedings will need to be issued on or before [date].
Please acknowledge this letter by [insert date 14 days after deemed receipt] and confirm to whom any Letter of Claim should be sent. We enclose a duplicate of the letter for your insurer.
Recoverable Benefits
The claimant’s National Insurance Number will be sent to you in a separate envelope.
We look forward to hearing from you.
Yours faithfully,
C2 Letter of Claim
To
Defendant
Dear Sirs
Letter of Claim
[Claimant’s name] –v- [Defendant’s Name]
We have been instructed to act on behalf of [Claimant’s name] in relation to treatment carried out/care provided at [name of hospital or treatment centre] by [name of clinician(s) if known] on [insert date(s)]. Please let us know if you do not believe that you are the appropriate defendant or if you are aware of any other potential defendants.
Claimant’s details
Full name, DoB, address, NHS Number.
Dates of allegedly negligent treatment
- include chronology based on medical records.
Events giving rise to the claim:
- an outline of what happened, including details of other relevant treatments to the client by other healthcare providers.
Allegation of negligence and causal link with injuries:
- an outline of the allegations or a more detailed list in a complex case;
- an outline of the causal link between allegations and the injuries complained of;
- A copy of any supportive expert evidence (optional).
The Client’s injuries, condition and future prognosis
- A copy of any supportive expert report (optional);
- Suggestions for rehabilitation;
- The discipline of any expert evidence obtained or proposed.
Clinical records (if not previously provided)
We enclose an index of all the relevant records that we hold. We shall be happy to provide copies of these on payment of our photocopying charges.
We enclose a request for copies of the following records which we believe that you hold. We confirm that we shall be responsible for your reasonable copying charges. Failure to provide these records may result in costs sanctions if proceedings are issued.
The likely value of the claim
- an outline of the main heads of damage, or, in straightforward cases, the details of loss;
- Part 36 settlement offer (optional);
- suggestions for ADR.
Funding
[State method of funding and whether arrangement was entered into before or after April 2013.]
We enclose a further copy of this letter for you to pass to your insurer. We look forward to receiving an acknowledgment of this letter within 14 days and your Letter of Response within 4 months of the date on which this letter was received. We calculate the date for receipt of your Letter of Response to be [date].
Recoverable Benefits
The claimant’s National Insurance Number will be sent to you in a separate envelope.
We look forward to hearing from you.
Yours faithfully
C3 Letter of Response
To
Claimant
Dear Sirs
Letter of Response
[Claimant’s name] –v- [Defendant’s Name]
We have been instructed to act on behalf of [defendant] in relation to treatment carried out/care provided to [claimant] at [name of hospital or treatment centre] by [name of clinician(s) if known] on [insert date(s)].
The defendant [conveys sympathy for the adverse outcome/would like to offer an apology/denies that there was an adverse outcome].
Parties
It is accepted that [defendant] had a duty of care towards [claimant] in respect of [details if required] treatment/care provided to [claimant] at [location] on [date(s)].
However, [defendant] is not responsible for [details] care/treatment provided to [claimant] at [location] on [date(s)] by [name of clinician if known].
Records
We hold the following records…
We require copies of the following records…
Failure to provide these records may result in costs sanctions if proceedings are issued.
Comments on events and/or chronology:
We [agree the chronology enclosed with the Letter of Claim] [enclose a revised chronology of events].
We enclose copies of relevant [records/Protocols/internal investigations] in respect of the treatment/care that [claimant] received.
Liability
In respect of the specific allegations raised by the claimant, the defendant [has obtained an expert opinion and] responds as follows:-
[each allegation should be addressed separately. The defendant should explain which (if any) of the allegations of breach of duty and/or causation are admitted and why. The defendant should also make clear which allegations are denied and why].
Next Steps
The defendant suggests…
[e.g. no prospect of success for the claimant, resolution without admissions of liability, ADR, settlement offer, rehabilitation].
Yours faithfully,”
Updated: Friday, 22 March 2024